Definition
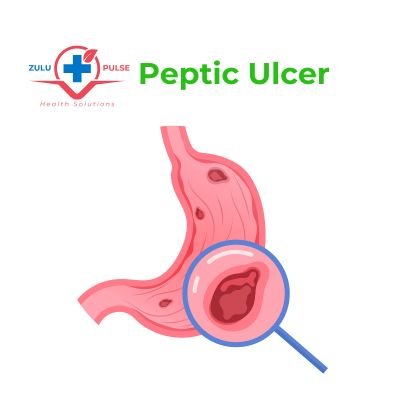
Peptic Ulcer Disease (PUD) is an ulceration of the gastric mucosa or duodenum, the first part of the small intestines. it can occur in rare cases in the oesophagus or jejunum after surgical anastomosis to the stomach.
Peptic ulcer disease may be acute or chronic depending on duration of symptoms and changes that occur in the lining of the stomach or duodenum. In Chronic PUD, there is evidence of fibrosis while in acute peptic ulcer disease it is not present.
The lifetime prevalence rate of peptic ulcer is between 5% to 10%. Ulcers may range in size from several millimeters to several centimeters. They can occur at any age but are more common in adults.
Gastric ulcer and duodenal ulcer share some of the symptoms but with some difference, treatment is also slightly different in terms of duration.
Causes of Peptic Ulcer Disease
The two main causes of peptic ulcer disease are infection with Helicobacter Pylori (H. Pylori) bacteria and nonsteroidal anti-inflammatory drugs (NSAIDs). There are some risk factors that increase risk of ulcer development as well.
Helicobacter Pylori Bacteria
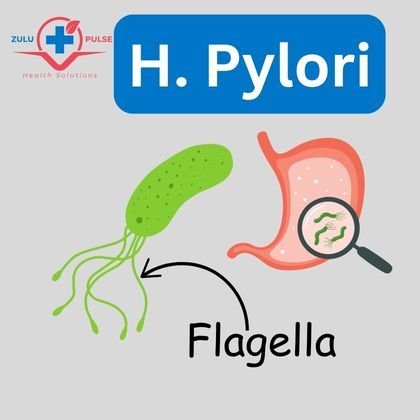
H. Pylori is a spiral urease producing bacteria that colonizes gastric mucosa. It is the cause of about 80% of cases of gastric ulcer and almost 100% of all duodenal ulcer cases. The infection affects 90% of the population in developing and underdeveloped countries (low socioeconomic status). The prevalence of H. Pylori infection is lower in high income countries. Infection is thought to spread from person to person through contact during childhood, majority of people remain asymptomatic.
The bacteria is gram negative with multiple flagella that helps it move (see the image below). H. Pylori produce enzyme urease which create ammonia from urea to neutralize the stomach acid around it so it can survive and invade the mucosa. The invaded part has chronic inflammation which later leads to apoptosis and formation of an ulcer.
Risk Factors
- Cigarette smoking
- Alcohol use
- Obesity
- Family history of ulcer
- Acid reflux Disease (GORD)
- Delayed gastric Emptying
- Zollinger-Ellison Syndrome
- Chronic atrophic gastritis
- Burns
Gastric Ulcer
Gastric ulcer occur in the stomach on the lesser curvature and mainly in elderly. If it occurs elsewhere it tends to be malignant.
Symptoms
- Epigastric pain radiating to the back described as burning or dull aching
- Pain may be relieved by antacids, sometimes worsened by eating
- Indigestion
- Weight loss
- Heart burn
- Vomiting
- Hematemesis
- Melena stool
Duodenal Ulcer
Duodenal ulcer is occurs in the first part of the small intestine in someone with peptic ulcer disease. Causes and risk factors are the same for both gastric ulcer and duodenal ulcer.
Symptoms
May be asymptomatic.
- Epigastric pain worsened by hunger and relived by food.
- Pain wakes you at night or in the early hours of the morning
- Occasional vomiting
- Melena stool
Investigations
The following investigations are done if Peptic ulcer disease is suspected.
1. H.Pylori infection tests
Helicobacter Pylori (H. Pylori) infection is the most common cause of PUD. There are several methods to confirm the infection, some are invasive while others are non-invasive. They also differ in sensitivity and specificity.
Non-invasive methods:
- Blood test: H. Pylori ELISA detects antibodies to the bacteria. It does not differentiate current infection from past infection. It is more than 90% specific and more than 80% sensitive.
- 13C-urea breath test: The test has sensitivity and specificity of more than 90%. It can be used as follow up test after treatment. It is also rapid and simple although it can be expensive.
- Stool antigen: The test also has high sensitivity and specificity or more than 90%. It is cheaper than breath tests but less convenient.
Invasive methods (Antral biopsy)
Invasive methods of testing H. Pylori infection involves biopsy of the stomach to perform one or more of the following tests:
- Histology: Histology is sensitive but takes several days to process
- Rapid Urease: The test is simpler but can yield false negatives if there is recent use of Proton Pump Inhibitors (PPIs), antibiotics or bismuth compounds in the past 4 weeks.
- Culture: Culture has advantage of identifying the specific antibiotic to treat the infection. Its disadvantage is that it is time consuming.
2. Endoscopy
Upper GI Endoscopy is recommended to confirm ulcer and biopsy to exclude malignancy especially in patients with ALARM signs.
ALARM Signs
- Iron Deficiency Anemia
- Loss of weight
- Age more than 55 years
- Recent onset or progressive symptoms
- Melena stools or hematemesis
- Swallowing difficulty (Dysphagia)
Treatment of Peptic Ulcer Disease
There are three main parts on approach to treatment of peptic ulcer disease, whether it’s gastric ulcer or duodenal ulcer:
- H. Pylori Eradication.
- Acid suppression with Proton Pump Inhibitors (PPIs).
- Remove cause or exacerbating factors e.g. NSAIDs.
H. Pylori Eradication
Eradication therapy of H. Pylori is with use of two antibiotics for at least 7 days to 10 days. For Adults:
- Amoxicillin 1g oral 12 hourly for 10 days AND
- Metronidazole 400mg oral 12 hourly for 10 days
In the case of Penicillin allergy, clarithromycin or azithromycin may be used to replace amoxicillin.
Gastric Acid Suppression
PPIs should be used together with antibiotics but for at least 14 days to 28 days. Choices of PPIs are:
- Lansoprazole 30mg oral daily, OR
- Omeprazole 20mg oral daily, OR
- Pantoprazole 40mg oral daily
Over-the-counter antacids such as Aluminium Hydroxide can be used. Patients with peptic ulcer disease should be told to avoid all NSAIDs and alcohol as that increase risk of upper GI bleeding and ulcer perforation.
Some patients may require chronic PPI use as maintenance. Lowest effective dose of PPIs should be used in consultation with specialist.
Complications
- Perforation
- Iron deficiency anemia
- Upper gastrointestinal (GI) bleeding
- Gastric cancer
- Gastric outlet obstruction