Definition
Atrial fibrillation (AF) is a type of cardiac arrhythmia where atrial rhythm of the heart is rapid and chaotic with irregularly irregular rhythm. It is one of the most common arrhythmias affecting 3 to 6 million adults in the United States alone.
AF is especially common in elderly affecting about 9% of the population. In most cases it remains asymptomatic. The main risk in atrial fibrillations is embolic stroke and reduced cardiac output which eventually becomes heart failure.
In atrial fibrillation, the atrial rate ranges between 300 and 600 beats per min. This is causes ventricles to also contract faster due to multiple stimulations but with decrease of cardiac output by about 10 to 20%.
It’s recommended to do an ECG on everyone with irregular pulse rhythm.
Causes of Atrial Fibrillation
- Hypertension
- Coronary artery disease
- Cardiomyopathy
- Valvular heart disorders such as mitral stenosis
- Heart failure
- Pulmonary Embolism (PE)
- Alcohol abuse
- Caffeine
- Hyperthyroidism
- Sleep apnea
- Pericarditis
- Myocarditis
- COPD
Clinical features
Atrial fibrillation can be asymptomatic until a complication such as Stroke occurs.
Symptoms
- Chest pain or discomfort on the central chest or left breast region
- Palpitations described as feeling like the heart is pounding hard or beating fast.
- Dyspnea
- Light headedness and dizziness
- Fainting
Some patients may present with symptoms of heart failure such as lower limb swelling, orthopnea, paroxysmal nocturnal dyspnea (PND), or shortness of breath on exertion.
Signs of Atrial Fibrillation
- Irregular irregular pulse. You should count the rate manually for the whole minute to get correct pulse rate in suspected AF
- Loss of waves in the JV pulse
- Apical pulse rate faster than radial pulse rate, a phenomenon called pulse deficit
- Eleveted Blood Pressure in the case of hypertension as the cause
- Signs of heart failure such as raised JVP, bipedal pitting oedema, pulmonary congestion etc.
It is important to examine the whole patients as additional signs pointing to the cause of AF may be present.
Diagnosis of AF
Atrial fibrillation diagnosis is made on an ECG. Additional tests are done to identify the cause and determine cardiac output.
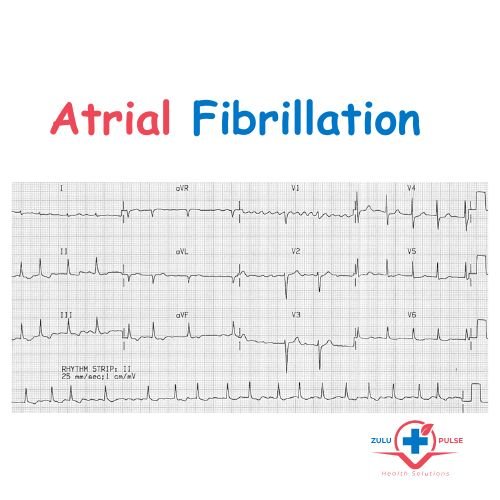
1. ECG
Electrocardiogram if recorded properly will have the following features:
- Absent P waves
- Presence of f waves between QRS complexes: commonly seen on V1 as irregular waves with rate >300bpm
- Irregularly irregular R-R interval
2. Echocardiogram
Echocardiogram is done to assess structure and functioning of the heart.
It is used to determine the cardiac output and rule out heart conditions that can cause AF (see above mentioned causes).
3. Blood Tests
These are done to rule out other medical conditions that are known to cause atrial fibrillation. These are:
- TSH and T4 to rule out thyroid disorders
- Lipid profile to asses coronary artery disease risk
- Full blood count (FBC)
- U&E
Treatment of Atrial Fibrillation
Atrial fibrillation treatment aim is to achieve the following:
- Rate control
- Prevention of thrombus formation and stroke with anticoagulants
- Rhythm control in younger patients, presenting for the first time or acute onset AF
- Treatment of complications and cause
Patients who are hemodynamically unstable need hospitalization. Synchronised Direct Current (DC) cardioversion is done starting at 120 to 15J. Amiodarone may be necessary as well. Consultation with specialist or experienced medical officer is necessary.
Rate control is done through use of ß-blockers, digoxin or amiodarone. The aim is to keep heart rate below 90bpm at rest. ß-blockers should not be given with verapamil as it is a rate limiting calcium channel blocker.
Rhythm control with elective DC cardioversion if the patient is not in failure
Anticoagulants are given if the patient has a CHA(2)DS(2)-Vasc score of ≥ 2 to prevent thromboembolic stroke. Warfarin is the preferred anticoagulant. Other additional medical conditions not mentioned on the score can also require use of anticoagulants.
These include Mechanincal artificial heart valve, hypertrophic cardiomyopathy and moderate to severe rheumatic mitral stenosis.
Patients on warfarin should be monitored frequently to maintain INR levels between 2-3. Conversion to sinus rhythm does not eliminate the need for chronic anticoagulants in patients who meet the criteria.
